Ovulation is the release of an egg from the ovary. Most women ovulate every month once they reach puberty. Ovulation then stops at menopause, when there are not enough eggs in the ovary for one to be released. If ovulation doesn’t occur, then the sperm has no chance of fertilising an egg to create an embryo and pregnancy just won’t happen so fertility is compromised.
Not releasing an egg from the ovary (not ovulating) can be the main fertility problem for some couples. Most of the time they can conceive without resorting to IVF. This article describes how you can assess ovulation and use medication to induce ovulation. We were also asked to write an article about how to induce ovulation for a magazine for general practitioners
There is more information on exercise on endocrinologytoday.com.au

How do I know if I am ovulating?
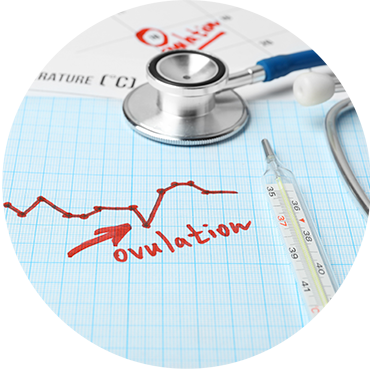
The best indicator of ovulation is having a regular period. When your cycles are between 25-35 days in length you are likely to be ovulating. If your cycles are less than 25 days or longer than 35 days in length, then you may not be getting the chance to conceive, as an egg may not be being released from the ovary. Other ways of assessing ovulation are:
- If you take your temperature daily first thing in the morning it will rise by half a degree after you have ovulated.
- The mucous at the neck of the womb (cervix) becomes transparent and very stretchy around ovulation when estrogen levels (a hormone produced by an egg that is close to ovulating) are high.
- Ovulation kits that you can buy from the chemist will detect the hormone that triggers ovulation (luteinising Hormone or LH) when you wee on them.
- A blood test taken 1 week after ovulation (on day 21 if you have a 28 day cycle) will detect a hormone called progesterone. This hormone is only secreted from the ovary after the egg has been released.
- We can formally track a menstrual cycle over a month using blood tests and scans. The blood tests measure the hormone changes that direct egg growth and ovulation. The scans can visualise the growing egg, check that the lining is thick enough for the embryo to implant and show that the egg has been released. We can also tell you when to try and conceive.
If it is difficult to detect the changes of ovulation, if your cycles are very irregular or if the ovulation kit sticks show a slight positive on or off or all the time, it is likely that you are not ovulating. It is a good idea to visit your general practitioner or a fertility specialist for advice as there are a lot of treatments for anovulation that help couples have a baby without needing IVF.
Why don’t some women ovulate when they want to have a baby?
There are lots of reasons women may not be ovulating including:
- They are stressed or under pressure
- They exercise and/or diet a lot and have a low body mass index
- They have an over or underactive thyroid gland
- They have a problem with their adrenal gland
- They are breastfeeding or have high levels of the hormone of breastfeeding
- They have polycystic ovarian syndrome (jeanhailes.org.au)
- They have too few eggs to ovulate
To investigate, we do some blood tests to work out why someone is not ovulating and we usually do tests to check how many eggs are in their ovaries as well. Depending on these blood tests, we sometimes have to use an an ultrasound or MRI machine to visualise the hormone producing glands (the pituitary, thyroid or adrenal gland).

How can we help you if you are not ovulating?
Firstly, we look check that hormones like the thyroid hormone or the hormone of breast feeding (prolactin) are not being over or under secreted. If they are, we can prescribe medications like thyroxine for a low thyroid or carbergoline for a high prolactin levels and that may be all we have to do to induce ovulation.
In others instances, we can use tablets like letrozole or clomiphene to tell the gland at the base of the brain (pituitary) to make more of the hormone that tells the ovary to grow eggs (follicle stimulating hormone or FSH). We initially use one table every day for 5 days in the early part of the menstrual cycle and do a scan and blood test 6 days later to see if an egg has grown. If not we increase the dose to 2 tablets a day then check again 6 days later. We start on a low dose and increase the dose slowly every 6 or so days to avoid getting too many eggs to grow. If you have too many eggs and try to conceive you could end up with too many pregnancies (the octo-Mum scenario!). If you have too many eggs then we have to cancel the cycle that month.
In Australia, the 2 medications we use are letrozole and clomiphene. Letrozole is newer, stays in the body for a shorter time and appeared to be slightly more effective in a recent review, so we often use it first. Clomiphene has helped many couples conceive over many years and for some women is a better medication. Both medications are given in the same way (for 5 days during the early part of the menstrual cycle).
When do I start medications if I rarely get a period?
We usually start medications like letrozole and clomiphene a few days after a period, but some women may not get a period for several months. In this situation, usually the hormone levels stay very flat over time, as they are not directing the ovulation process. If the hormone levels are always the same as they would be just after a period, the letrozole and clomiphene can be started at any time as long as a blood test has been done to ensure there is not other reason for not having a period ( like being pregnant!).
If you haven’t had a period for a long time the lining of the womb may slowly but surely become thicker and thicker, and an embryo would find it difficult to implant. We can induce a period if the lining is too thick, by prescribing a hormone called progesterone. To induce a period you take progesterone for 7-10 days then stop it. A period will start 7-10 days after stopping the progesterone.


When is Metformin used?
When women have polycystic ovarian syndrome they often also have high insulin levels in the blood (diabetes.diabetesjournals.org). We don’t know how but insulin seems to act as a block to ovulation and Metformin acts to lower insulin levels. A recent review indicated that Metformin with Clomiphene was better than only Clomiphene in the treatment of anovulation (www.bmj.com). There is also some evidence that Metformin may reduce the risk of miscarriage for some women with high insulin or sugar levels.
What if tablets don’t work?
Sometimes women don’t have enough follicle stimulating hormone (FSH) in the pituitary gland in the base of the gland to tell the ovaries to make eggs, even if we give them medications like letrozole or clomid. They often also have a low hormone called luteinising hormone or LH which triggers the release of the egg by the ovary. Often these hormones are low if women exercise or diet a lot and they have a low body mass index but sometimes we don’t know why they are low.
In this situation we ‘become the pituitary gland’ and prescribe FSH injections to make the eggs grow. We give these injections daily just under the skin via a special drug pen using very, very fine needles (if ice is placed on the lower abdominal or upper leg skin before the injection it doesn’t hurt too much). FSH is a very powerful medication so its use needs to be carefully monitored as there is a much higher risk of multiple pregnancy. We need to monitor closely with scans and blood tests. We also sometimes have to trigger the release of the egg by giving an injection of hCG (a long acting form of LH) as well as 1-2 injections after ovulation to tell the ovary to keep making hormones like progesterone to keep the lining of the womb ready for implantation.
Another treatment to induce ovulation, which we are using less and less often is laparoscopy and making small holes in the ovary (ovarian drilling). We are still unsure how it works and we would only consider it if there someone had high ovarian reserve usually with polycystic ovarian syndrome, but it is still used and can help the release of eggs from the ovary or help the other medications that induce ovulation work better.


Is IVF an option?
IVF is an option and sometimes it is the only way to help couples with ovulation problems. Sometimes there is an all or nothing response to the ovulation medications we use, where either none of the eggs grow or lots of eggs (15 or more) grow. If there are always a high number of eggs rather than cancelling cycles repeatedly, we can remove the eggs from the body and do IVF and we really want about 15. We can convert an ovulation induction cycle to IVF if there are too many eggs to give a couple a chance of pregnancy and we may get frozen embryos as well. Another reason we may use IVF to treat couples with ovulation problems is when there is another fertility issue such as a low sperm count and we can improve fertilisation in the lab.

Ovulation problems are often a cause of reduced fertility, however we do have good ways of inducing ovulation, often with tablets. Recognising and diagnosing the reason why someone isn’t ovulating is critical as there are many simple treatments that will help conception that don’t require IVF. Understanding the biology of ovulation and tailoring treatment to induce ovulation is an important part of a fertility specialist’s job. It is great when a simple change of medication or lifestyle helps a couple have a baby without needing intensive treatments like IVF.




